

A covered entity must provide individuals (or their personal representatives) with access to their own PHI (unless there are permitted grounds for denial), and must provide an accounting of the disclosures of their PHI to others, upon their request.A HIPAA-compliant Authorization must contain specific information required by the Privacy Rules. as authorized by the person (or personal representative) who is the subject of the health information.as the Privacy Rule permits or requires or.Generally, a covered entity may not use or disclose PHI to others, except: A major purpose of the Privacy Rule is to define and limit the circumstances under which an individual's PHI may be used or disclosed by covered entities.The Privacy Rule protects all “ protected health information” ( PHI), including individually identifiable health or mental health information held or transmitted by a covered entity in any format, including electronic, paper, or oral statements.
Covered entities include almost all health and mental health care providers, whether they are outpatient, residential or inpatient providers, as well as other persons or organizations that bill or are paid for health care. The Privacy Rule applies to “ covered entities” which generally includes health plans and health care providers who transmit health information in electronic form. The Rule is intended to provide strong legal protections to ensure the privacy of individual health information, without interfering with patient access to treatment, health care operations, or quality of care. The HIPAA Privacy Rule (45 CFR Parts 160 and 164) provides the first comprehensive Federal protection for the privacy of health and mental health information.

State statutes which provide more stringent protections of health care privacy remain in effect even after HIPAA, and therefore this document includes a few relevant references to requirements in New York State's mental health confidentiality statute (section 33.13 of the Mental Hygiene Law). HIPAA required the federal Department of Health and Human Services ( HHS) to develop regulations to implement these privacy requirements, called the Privacy Rule, which became effective on April 14, 2003.
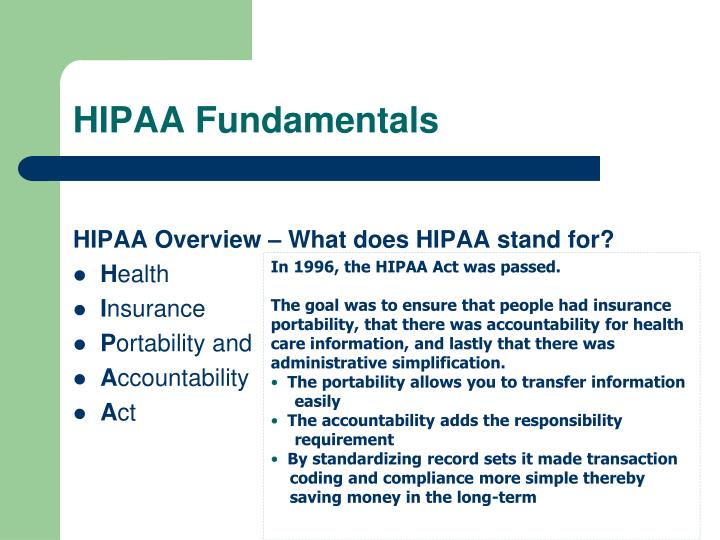
This document provides guidance about key elements of the requirements of the Health Insurance Portability and Accountability Act ( HIPAA), federal legislation passed in 1996 which requires providers of health care (including mental health care) to ensure the privacy of patient records and health information. Mental health providers and other covered entities should not rely on this summary as a source of legal information or advice and should consult with their own attorney or HIPAA Privacy Officer for specific guidance.) This web site has been developed to give you the resources required to ensure that Emory remains compliant with federal laws and regulations.(Note: The information provided below is a summary and intended for general informational purposes. Everyone at Emory must consider how health information should be handled and protected. The Emory Covered Entity has developed high level security policies and will undertake employee training to ensure that all information is appropriately disseminated. The important thing to remember is that every medical entity in the United States is required to comply with these regulations. These HIPAA rules and standards will create major changes in the way the Emory Covered Entity functions.
#Hipaa stands for code
There are three separate sets of rules affecting the Emory Covered Entity that cover standardization of healthcare transactions and code sets, the Privacy Rule which includes new rights for patients regarding their personal health information, and the Security Provision detailing the specific technology security protections all health care organizations must undertake to ensure confidentiality of patients' medical information. HIPAA stands for the Health Insurance Portability and Accountability Act which was signed into law in 1996.


 0 kommentar(er)
0 kommentar(er)
